Why Does Pain Happen in hEDS?
Compensatory Muscle Engagement & Myofascial Spasm
Central Sensitization & Widespread Pain
Ongoing pain signals from unstable joints can trigger central sensitization in the nervous system, causing widespread pain that extends beyond the original site. This “amplification” of pain is well-documented in hEDS, with enhanced pain responses confirmed in research (Di Stefano et al., 2016; De Wandele et al., 2022).
Impaired Proprioception & Muscle Weakness
Reduced proprioceptive feedback (your body’s sense of joint position) and muscle weakness force the body to rely even more on compensatory strategies, perpetuating the pain and instability cycle (Syx et al., 2017).
What Works for Pain in hEDS?
Pain Neuroscience Education (PNE)

Combining pain neuroscience education with exercise is supported by moderate-quality evidence for reducing pain and improving function in chronic musculoskeletal conditions, and emerging research shows specific benefit in hEDS. PNE helps you understand how pain works, reduces fear of movement, and empowers you to break the pain cycle. Notably, programs that include pain education have shown significant improvements in pain, pain-related disability, and kinesiophobia (fear of movement) in hEDS (Celletti et al., 2021; Chew et al., 2025; Siddall et al., 2022).
Proprioceptive Training
Proprioceptive training (exercises that enhance your awareness of joint position and movement) consistently improves balance, confidence, and quality of life in hEDS. Comprehensive rehab programs that include proprioceptive and motor function training produce lasting improvements in exercise capacity, balance, and daily function (Reychler et al., 2021; Garreth Brittain et al., 2024; Hakimi et al., 2023). At TCS, we integrate proprioceptive training into every treatment plan, tailoring activities to your unique needs and goals.
Biofeedback and Parasympathetic Activation
While direct evidence is still emerging, biofeedback is a promising tool for helping clients engage deep stabilizing muscles and develop greater body awareness. Parasympathetic activation techniques, such as nervous system drills, breathwork, and vagus nerve activities, have demonstrated significant improvements in mental quality-of-life and pain reduction. These low-risk, practical strategies are routinely included in our OT sessions to support nervous system regulation and decrease neuroplastic (central) pain (Lattimore & Harrison, 2023).
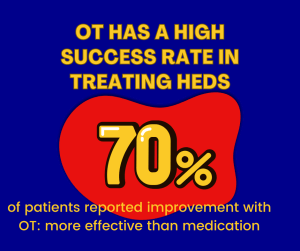
Multidisciplinary & Occupational Therapy Interventions
- Environmental modifications: Adapting home and work spaces to reduce strain, conserve energy, and support safe movement (e.g., ergonomic workstations, wide-grip utensils, suitable mattresses, mobility aids) (Hakim, 2024; Minhas, 2021; Yew et al., 2021).
- Self-management strategies: Education on pacing, joint protection, and activity modification tailored to your daily life.
- Assistive devices: Recommendations for wheelchairs, scooters, soft collars, and other supports as needed.
- Enablement and behavioral change: Clients consistently prioritize OT-led adaptations and practical support as the most important interventions for maintaining independence (Bennett et al., 2022).
Why TCS?
TCS’s OT team is committed to evidence-based, client-centered care. We blend pain neuroscience education, proprioceptive and motor training, environmental enablement, and nervous system regulation into every plan. Our approach is practical, flexible, and always tailored to your needs—because living well with hEDS is possible, and you deserve support that works.
